UZAYAN KOVİD

Dikkat: Yazının sonunda ek var!
***
İndependent Türkçe‘ deki yazım:
KOVİD’ i yakın zamanlara kadar başlıca dört klinik tabloda tanımlıyorduk:
BİR: Hiçbir hastalık belirtisi vermeyen KOVİD (asemptomatik vakalar)
İKİ: Tıbbi yardım almaya ihtiyaç kalmadan hafif ve kısa zamanda da geçen belirtilerle seyreden KOVİD
ÜÇ: Hastaneye yatırılmayı gerektirmeyen ama ilaç tedavisi icap eden KOVİD
DÖRT: Hastaneye ve yoğun bakıma yatırılmayı gerektiren ağır ve ölüm riski yüksek KOVİD.
Uzayan KOVİD
Hasta sayıları arttıkça bunlara yeni bir tablo daha eklendi: Uzayan KOVİD.
Bu klinik tablo nispeten hafif akut hastalıktan sonra ortaya çıkan ve birçok sistemi tutan bir hastalık olarak kabul ediliyor.
İngilizce literatürde post-akut KOVİD veya long KOVİD gibi isimler verilen bu hastaların çoğu ayaktan tedavi edilmiş olmakla beraber içlerinde hastanede yatmış olanlar da bulunabilir. 1
Bu tabloyu çok ağır hastalık geçiren ve akciğer, kalp, sinir sistemi ve böbrekler gibi hayati organlarda birtakım hasarlar kalan, dolayısıyla da iyileşmeleri uzun zaman isteyen veya tam düzelmesi beklenmeyen hastalarla karıştırmamak gerekir.
Akciğerlerinde fibrozis yani bağ dokusu artışı gelişen hastaların veya yaygın damar içi pıhtılaşması yaşayanların şikayetlerinin çok uzun süre hatta ömrü boyu sürmesi mümkündür.
Mesela İtalya’da hastaneye yatırılan 143 hasta üzerinde yapılan bir araştırmanın da gösterdiği gibi taburcu olduktan 2 ay sonra yüzde 87’si en azından yorgunluk ve nefes darlığı şikayetlerinden biri devam eden hastalar uzayan KOVİD kapsamı dışında kabul edilmelidir. 2
Hastaların çoğu iki haftada düzeliyor
KOVİD, çoğu hastada ilk belirtiler ortaya çıktıktan iki hafta sonra tamamen düzeliyor; ama bazı vakalarda bu süre uzayabiliyor.
Uzayan KOVİD teşhisi için gereken süre hakkında bir fikir birliği yok; belirtilerin akut dönemden üç hafta sonra da devam etmesini yeterli bulanlar olmakla beraber ben bu sürenin altı hafta olmasını kabul edenlere katılıyorum.
Nitekim ABD’de yapılan yeni bir çalışma, insanların sadece yüzde 65’inin pozitif bir testten 14-21 gün sonra önceki sağlık seviyelerine geri döndüğünü gösteriyor. 3
Hastaların, bir akıllı telefon uygulamasına devam eden şikayetlerini kaydetmeleri suretiyle yürütülen UK COVID Symptom Study isimli araştırmaya göre uzayan KOVİD, testleri pozitif her 10 KOVİD hastasından birinde görülüyor.
Bu çalışma, Birleşik Krallık’ta 300 bin kadar kişide bir aydan uzun süredir, 60 bin kişide ise 3 aydan uzun süredir devam eden belirtiler olduğunu gösteriyor. 4
Gözleme dayalı birçok araştırmada bundan çok daha yüksek oranlar da bildiriliyor; ama bunlarda vakaların kaynağının hastanede yatan veya özel kliniklere başvuranlar olduğuna dikkat etmek gerekir. 5, 6
Vakalarının çoğuna test yapılmamış olduğundan ve yanlış negatif neticeler sık olduğundan uzayan KOVİD teşhisi için pozitif bir KOVİD testi şart koşulmuyor.
Neden bazı kişiler daha çok etkileniyor?
İyileşmenin bazı kişilerde neden uzadığı tam olarak bilinmiyor.
Antikor cevabının zayıf olması veya hiç olmaması, hastalığın nüks etmesi veya yeniden enfekte olmak, enflamatuar ve diğer bağışıklık tepkileri, kondisyon kaybı ve post-travmatik stres gibi mental faktörler üzerinde duruluyor.
Uzayan KOVİD kadınlarda erkeklere göre iki kat fazla görülüyor.
Uzayan KOVİD’ in klinik tablosu
Uzayan KOVİD belirtileri hastadan hastaya değişiyor. Öksürük ve hafif ateşten baş ağrısına, koku alma kaybından yorgunluğa kadar çeşitli belirtiler bazı kişilerde sürekli olurken bazılarında ise alevlenmeler şeklinde görülüyor.
Bu uzayan hastalık belirtileri insanların hayatını ciddi şekilde etkiliyor.
Bazı hastalar ise göğüste baskı hissi, çarpıntı, kas ve eklem ağrıları, deri döküntüleri, ishal, uyuşma ve iğnelenme gibi belirtiler tarif ediyorlar.
Uzayan KOVİD hastası olan profesör Paul Garner, bu tabloyu “İlk iki ayda insanı adeta hırpalayan, sonraki dört ayda ise daha seyrek ataklara yol açan çok tuhaf bir hastalık” olarak tanımlıyor.
COVID Symptom Study‘nin başı olan profesör Tim Spector ise, “İlk haftada sürekli öksürük, ses kısıklığı, baş ağrısı, ishal, iştahsızlık ve nefes darlığı olanlarda belirtilerin uzun süre devam etme ihtimali 2-3 misli fazla” diyor. 7
Uzayan KOVİD’ in tedavisi holistik tıptır
Modern tıbba göre bu hastaların çoğunun yavaş da olsa holistik destek, istirahat, semptomatik tedavi ve aktivitenin tedrici olarak artırılmasıyla iyileştirilebilecekleri kabul ediliyor; ama içlerinde şikayetleri tüm bunlara rağmen bir türlü düzelmeyenler de vardır. 1
Holistik tıp, insanı ruh ve bedeni ile bir bütün olarak ele alıp tedavi etme sanatı olarak tarif edilir, bütüncül tıp diye de bilinir ve zaten olması gereken de budur.
Yeni bir çalışma da bu dönemde geçen seneye göre anksiyete ve depresyonda ciddi artış olduğunu, ruhsal yardım hattından yardım aramanın yüzde 65 arttığını ortaya koyuyor. 8
Ben de uzayan KOVİD vakalarında esas meselenin ruhsal olduğunu ve hastaların hem bedenine hem ruhlarına dokunulması gerektiğini düşünüyorum.
Gelelim neticeye
Aylardır süren, dünya çapında nerdeyse bir milyona yakın insanın hayatına mâl olan, giderek yavaşlamak bir tarafa alevlenmelerle seyreden ve ikinci bir dalgadan ciddi endişe duyulan, hâlâ bir ilaç ve aşısı olmayan KOVİD herkesin sosyal ve şahsi hayatını allak bullak etti.
Uzayan KOVİD’i hiç şüphe yok ki bundan sonraki dönemde çok daha fazla konuşacağız ve kim bilir daha neler öğreneceğiz, nelerle karşılaşacağız.
Şu an için tespitlerim şunlar:
BİR: Uzayan KOVİD’ in vücutta ciddi hasarlara yol açmış kronik KOVİD’ le karıştırılmaması çok önemli; çünkü bu ikinci grup hastaların belirtilerin mahiyetine göre pnömolog, kardiyolog, nörolog, nefrolog gibi mütehassıslar tarafından takip ve tedavi edilmeleri gerekiyor.
İKİ: Uzayan KOVİD hastalarının homojen bir grup olmadığı aşikârdır ve içlerinde gerçekten modern tıbba ihtiyaç duyanlar da vardır; ama ben bu vakaların büyük çoğunluğunun ruhsal kökenli olduğu kanaatindeyim.
ÜÇ: Uzayan KOVİD’ in tedavisinin de ilaçlarla değil, insanlara moral aşılayarak ve güçlü bir maneviyatla mümkün olacağına inanıyorum.
Kaynaklar:
1. https://www.bmj.com/content/370/bmj.m3026
2. https://jamanetwork.com/journals/jama/fullarticle/2768351
3. https://www.cdc.gov/mmwr/volumes/69/wr/mm6930e1.htm
4. https://www.bbc.com/news/health-54031587
5. https://publichealth.jmir.org/2020/2/e19462/
6. https://jamanetwork.com/journals/jama/article-abstract/2768351
7. https://www.bmj.com/content/370/bmj.m3489
8. https://www.nytimes.com/2020/09/07/health/coronavirus-mental-health-long-hauler.html
Kaynak: https://www.indyturk.com/node/242686/t%C3%BCrkiyeden-sesler/uzayan-kovid
***
EK 1 (14.9.2020): The lasting misery of coronavirus long-haulers. Kaynak: https://www.nature.com/articles/d41586-020-02598-6
***
EK 2 (18.11.2020): Yorgunluk, nefes darlığı, göğüs ağrısı, organ fonksiyon bozuklukları gibi belirtilerin sebebi virüsün doğrudan dokulara yayılması, immun sistem hasarı, pıhtılaşmanın artması veya bunların birlikte etkilerinden olabilir.
Kaynak: https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2020.19719
***
EK 3 (7.12.2021): “Uzayan Kovid’ den mustarip olduklarını iddia eden 27 bin katılımcı üzerinde yapılan Fransız araştırmasında, sadece yüzde 4’ünün önceden virüsle karşılaştığı tespit edildi. Kaynak: https://twitter.com/korcanayata/status/1467938493376643075?s=20
***
EK 4 (29.1.2022): HALUK VAHABOĞLU “long-covid korku yayıcıların uydurduğu çok çok ender bir durumdur” Long-covid ne yahu. Post covid komplikasyonlara verilen tamamen uygunsuz bir isim. Amaç korku salmak“
Kaynak: https://twitter.com/HalukVAHABOLU/status/1487240690425868288?s=20&t=np-EsOUXuGJxWB5ksdbL3g
***
EK 5 (31.5.2022): Kapsamlı değerlendirmelerde, çoğu vakada belirtilerin sebepleri ortaya konamadı. Anormal sistemik immün aktivasyon veya kalıcı viral enfeksiyona ait delil bulunamadı. Antikor seviyeleri çok değişkendi. Uzayan Kovid’ in patogenezi belli değildir.
Kaynak: https://www.acpjournals.org/doi/10.7326/M21-4905
Makale adı: A Longitudinal Study of COVID-19 Sequelae and Immunity: Baseline Findings
***
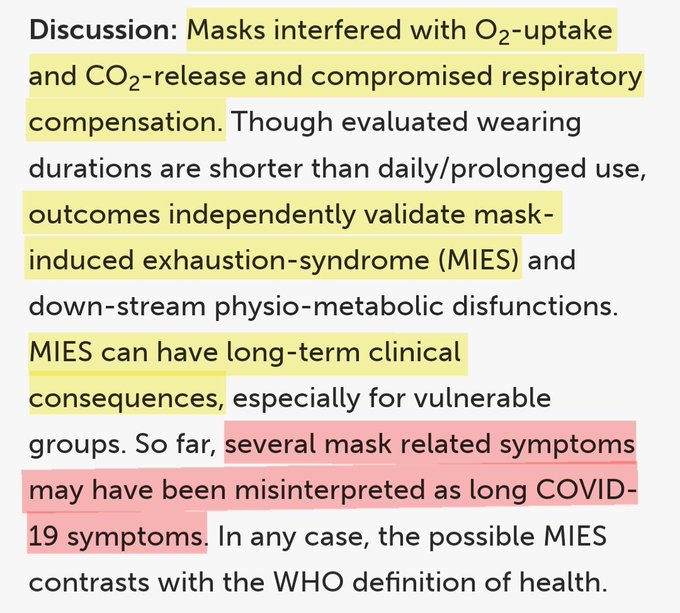
EK 6 (13.8.2022): BROWNSTONE INSTİTUTE “Mikroplastiklere, nanopartiküllere, maskelerdeki kimyasallara ve nazofaringeal testleredaha çok maruz kalma, Uzayan Kovid’ i tanımlayan semptomların çoğuna paraleldir.”
Kaynak: https://twitter.com/brownstoneinst/status/1558031118661722113
***
EK 6 (25.8.2022): Uzayan Kovid diğer post-viral durumlara benziyor.
Kaynak: https://www.medscape.com/viewarticle/979690
Makale: Long COVID Mimics Other Post-Viral Conditions
***
EK 7 (3.12.2022): Association of Initial SARS-CoV-2 Test Positivity With Patient-Reported Well-being 3 Months After a Symptomatic Illness
In this study, participants in both the COVID-19–positive and COVID-19–negative groups reported persistently poor physical, mental, or social well-being at 3-month follow-up. Although some individuals had clinically meaningful improvements over time, many reported moderate to severe impairments in well-being 3 months later. These results highlight the importance of including a control group of participants with negative COVID-19 results for comparison when examining the sequelae of COVID-19.
Kaynak: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2799116
***
EK 8 (11.12.2022): An early and influential paper on long COVID that appeared in The Lancet has been flagged with an expression of concern while the journal investigates “data errors” brought to light by a reader.
An editorial that accompanied the paper when it was published in January of last year described it as “the first large cohort study with 6-months’ follow-up” of people hospitalized with COVID-19. The article has received plenty of attention since then.
Titled “6-month consequences of COVID-19 in patients discharged from hospital: a cohort study,” the paper has been cited nearly 1,600 times, according to Clarivate’s Web of Science. Altmetric finds references to it in multiple documents from the World Health Organization.
According to the expression of concern, dated November 24, a reader found inconsistencies between the data in the article and a later paper describing the same cohort of patients after a year of follow-up. That discovery sparked an investigation that is still ongoing:
On Jan 8, 2021, The Lancet published an Article, 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study, by Chaolin Huang and colleagues.1 On Aug 28, 2021, The Lancet published an Article, 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study, by Lixue Huang and colleagues.2 We received an inquiry from a researcher on data inconsistencies between these two Articles, and we sought an explanation from the corresponding author of the two papers. On Nov 7, 2022, Lancet editors were informed that inconsistencies between the 6-month and the 1-year data were due to “some variables in the dataset used for the 6-month paper were mistakenly disrupted in order”. In view of the extent of these data errors, we now issue an Expression of Concern about the 6-month paper1 while we investigate further, including further statistical and clinical review of the corrected data. We will update this notice as soon as we have further information.
The corresponding author of both papers, Bin Cao of China’s National Center for Respiratory Medicine and the China-Japan Friendship Hospital in Beijing, has not responded to our request for comment.
A profile of Cao published in Lancet Infectious Diseases last March described him as “a leading researcher in pneumonia and influenza” who “has been instrumental in increasing knowledge about COVID-19.” In addition to the follow-up study of hospitalized COVID patients:
Cao’s seminal papers during the COVID-19 pandemic include the first report of the clinical characteristics of COVID-19 patients in Wuhan, the description of the risk factors for mortality for adult inpatients, and the results of trials testing the use of antiviral drugs, including lopinavir-ritonavir, to treat COVID-19 in China.
We reached out to The Lancet’s press office and Richard Horton, the journal’s editor-in-chief, and received this statement:
The Lancet Group treats all communications between editors and authors or readers as confidential. Investigations are continuing, and the Expression of Concern will be updated as soon as we have further information to share. More information about our policies is available here: https://www.thelancet.com/publishing-excellence
This year, The Lancet overtook the New England Journal of Medicine as the medical journal with the highest impact factor, in large part due to the papers it published about COVID-19.
We’ve counted retractions for three of those papers, most notably a paper about the use of the drug hydroxychloroquine that claimed to use medical data from a company called Surgisphere. As Retraction Watch readers may remember, the article was retracted after sleuths questioned if the data were real, and the company would not produce it for review.
***
EK 9 (13.12.2022): Long COVID is a poorly defined entity that is almost certainly a mix of real post-viral syndrome, psychosocial expectations, and secondary gain, mixed with the rate at which “stuff happens” that coincided w a ubiquitous viral infection.
There is a there, there, but the way we have gone about hyping it while not really defining it has made the research of seeing if there is anything different about COVID vs other coronaviruses very challenging.
Kaynak: https://twitter.com/davidemccune/status/1602538170926923776?s=20&t=6ACGC-BM1lgCU014_yiiiw
***
EK 10 (18.1.2023): The Exaggeration of Long Covid. Lingering symptoms after a respiratory infection are common. Most cases are too mild to worry about.
MARTY MAKARY “Hasta ve hareketsiz kaldıktan ve iyi beslenmedikten sonra haftalarca hafif yorgunluk veya halsizlik yaşamak genellikle normaldir. Bu vakalara uzun COVID demek, modern yaşamın tıbbileştirilmesidir,”
Kaynak: https://www.medscape.com/viewarticle/986969
Makale: Add This to the List of Long COVID Symptoms: Stigma
***
EK 11 (7.2.2023): Kovid’den önce sağlıklı hayat tarzı uzayan Kovid riskinin azalmasıyla ilişkili bulundu.
Makale: Adherence to Healthy Lifestyle Prior to Infection and Risk of Post–COVID-19 Condition
Kaynak: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2800885
***
EK 12 (31.3.2023): The persistent symptoms and disability that characterize PCC are associated with factors other than SARS-CoV-2 infection, including psychosocial factors. This finding raises questions about the utility of the World Health Organization case definition and has implications for the planning of health care services as well as for further research on PCC.
Kaynak: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2802893
Makale: Prevalence and Characteristics Associated With Post–COVID-19 Condition Among Nonhospitalized Adolescents and Young Adults
***
EK 13 (11.4.2023):Long Kovid (Uzayan Kovid) aslında maske takmanın bir neticesi olabilir.
Kaynak: https://twitter.com/drahmetrasim/status/1645907720929943552?s=20
***
EK 14 (6.6.2023): Kovid enfeksiyonundan önce kaygı ve depresyona sahip olmak uzayan Kovid riskini artırıyor. Bir enfeksiyondan sonra anksiyete ve depresyon geliştiren uzayan Kovid’ li kişilerde beyin bağlantısının bozulmasının yanı sıra hafıza, duygu ve diğer işlevleri düzenleyen alanlarda beyin küçülmesi olabilir.
Kaynak: https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2796097
Makale: Associations of Depression, Anxiety, Worry, Perceived Stress, and Loneliness Prior to Infection With Risk of Post–COVID-19 Conditions
***
EK 15 (9.6.2023): Ucuz, güvenli ve yaygın olarak bulunabilen bir diyabet ilacı olan metformin, Kovid-19’un akut fazında verildiğinde uzayan Kovid insidansını azaltabiliyor.
Kaynak: https://www.bmj.com/content/381/bmj.p1306
Makale: Covid-19: Metformin reduces the risk of developing long term symptoms by 40%, study finds
Kaynak: https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(23)00299-2/fulltext
Makale: Outpatient treatment of COVID-19 and incidence of post-COVID-19 condition over 10 months (COVID-OUT): a multicentre, randomised, quadruple-blind, parallel-group, phase 3 trial
***
EK 16 (9.6.2023): Yeni yapılan bir araştırma, uzun süre devam eden COVID-19 (uzun COVID) hastalığıyla ilişkilendirilen 200 kadar belirtinin çoğunu eledi, esasen 12 belirti olduğunu gösterdi.
Araştırmacılar yıllardır uzun COVID’in tam olarak ne olduğunu tanımlamaya çalışıyor. Yeni yapılan bir çalışma, uzun COVID ile ilişkili olduğu düşünülen çok sayıda belirtiyi eleyerek, tam olarak bu hastalıkla ilişkili 12 belirtiyi netleştirdi. Daha önce 200 farklı belirtinin bu gizemli ve geçmeyen sağlık sorunuyla ilişkili olduğu düşünülüyordu.
COVID-19 küresel bir sağlık krizi haline geldiğinden bu yana, hastalıkla ilişkili kronik ve uzun vadeli etkilere dair raporların sayısı artıyor. Uzun COVID belirtileri arasında “beyin sisi”, yorgunluk, koku kaybı ile orta ve yüksek şiddette bazı diğer sorunlar yer alıyor.
Uzun COVID teşhisi koymanın zorlukları
Uzun COVID tanısı konması için tek kriter var, o da enfeksiyondan 30 gün sonrasında ve devamında süren, geri gelen veya yeni ortaya çıkan belirtilerin bulunması.
Dünya Sağlık Örgütü ( DSÖ), uzun COVID ile ilişkili olduğunu düşündüğü 200 farklı belirtiyi sıralıyor. Ancak bu koşullar altında, eğer bir teşhis sistemi kurulacaksa araştırmacıların uzun COVID hakkında daha net bilgilere sahip olması gerekiyor.
Uzun COVID ile ilişkili 12 belirti
ABD’den bir grup araştırmacı bu amaçla 8.646’sı daha önce COVID-19 geçiren, 1.118’i hiç bu hastalığı geçirmemiş olan bir kontrol grubu olmak üzere yaklaşık 10.000 kişilik bir gruba ait verileri inceledi. Gruptaki her bir kişiyle anket yapıldı ve en çok bildirilen belirtilerin listesini oluşturuldu. Bu sayede belirtilerin her birinin COVID-19 ile ne kadar ilişkili olduklarına göre puan verildi.
Sonuçlar, uzun COVID ile ilgili en sık görülen belirtilerden 12’sini ortaya çıkardı. Listenin ilk sırasında 8 puan ile, COVID-19’un karakteristik bir semptomu olan koku veya tat kaybı var. İkinci sırada “efor sonrası halsizlik” (fiziksel veya zihinsel egzersizden sonra yorgun hissetme), üçüncü sırada kronik öksürük yer alıyor.
2. ve 3. sıradaki belirtiler arasında büyük bir puan var. Bu da ilk iki semptomun diğerlerine göre daha yaygın ve uzun COVID-19 ile ilişkili olma olasılığının daha yüksek olduğunu gösteriyor.
Belirtiler şu şekilde sıralanıyor:
Belirti (puan)
- Koku/tat (8)
- Efor sonrası halsizlik (7)
- Kronik öksürük (4)
- Beyin sisi (3)
- Susuzluk (3)
- Çarpıntı (2)
- Göğüs ağrısı (2)
- Yorgunluk (1)
- Cinsel istek veya kapasite (1)
- Baş dönmesi (1)
- Sindirim sistemi (1)
- Anormal hareketler (1)
- Saç dökülmesi (0)
Kaynak: https://www.gidahatti.com/haber/15247629/uzun-covid-belirtileri-200den-12ye-indi
Makale: Development of a Definition of Postacute Sequelae of SARS-CoV-2 Infection
Kaynak: https://jamanetwork.com/journals/jama/fullarticle/2805540
***
EK 17 (4.7.2023): Rare link between coronavirus vaccines and Long Covid–like illness starts to gain acceptance Studies probe unusual cases of neurologic complications, blood pressure swings, and other side effects
COVID-19 vaccines have saved millions of lives, and the world is gearing up for a new round of boosters. But like all vaccines, those targeting the coronavirus can cause side effects in some people, including rare cases of abnormal blood clotting and heart inflammation. Another apparent complication, a debilitating suite of symptoms that resembles Long Covid, has been more elusive, its link to vaccination unclear and its diagnostic features ill-defined. But in recent months, what some call Long Vax has gained wider acceptance among doctors and scientists, and some are now working to better understand and treat its symptoms.
“You see one or two patients and you wonder if it’s a coincidence,” says Anne Louise Oaklander, a neurologist and researcher at Harvard Medical School. “But by the time you’ve seen 10, 20,” she continues, trailing off. “Where there’s smoke, there’s fire.”
Cases seem very rare—far less common than Long Covid after infection. Symptoms can include persistent headaches, severe fatigue, and abnormal heart rate and blood pressure. They appear hours, days, or weeks after vaccination and are difficult to study. But researchers and clinicians are increasingly finding some alignment with known medical conditions. One is small fiber neuropathy, a condition Oaklander studies, in which nerve damage can cause tingling or electric shock–like sensations, burning pain, and blood circulation problems. The second is a more nebulous syndrome, with symptoms sometimes triggered by small fiber neuropathy, called postural orthostatic tachycardia syndrome (POTS). It can involve muscle weakness, swings in heart rate and blood pressure, fatigue, and brain fog.
Patients with postvaccination symptoms may have features of one or both conditions, even if they don’t meet the criteria for a diagnosis. Both are also common in patients with Long Covid, where they’re often attributed to an immune overreaction.
Although more researchers are now taking Long Vax seriously, regulators in the United States and Europe say they have looked for, but have not found, a connection between COVID-19 vaccines and small fiber neuropathy or POTS. “We can’t rule out rare cases,” says Peter Marks, director of the U.S. Food and Drug Administration’s Center for Biologics Evaluation and Research, which oversees vaccines. “If a provider has somebody in front of them, they may want to take seriously the concept [of] a vaccine side effect,” he says. But Marks also worries about “the sensational headline” that could mislead the public, and he emphasizes that vaccine benefits far outweigh any risks.
Despite the uncertainties, German Minister of Health Karl Lauterbach acknowledged in March that though rare, Long Covid–like symptoms after vaccination are a real phenomenon. He said his ministry was working to organize funding for studies, although none has been announced so far.
Researchers studying these complications also worry about undermining trust in COVID-19 vaccines. Harlan Krumholz, a cardiologist at Yale University, says concern that the antivaccine movement would seize on any research findings made him hesitant at first to dive in. But about a year ago he and Yale immunologist Akiko Iwasaki began to welcome postvaccination patients into a new study called LISTEN that also includes Long Covid patients. Among other things, it aims to correlate symptoms with immune cell patterns in blood samples.
“I’m persuaded that there’s something going on” with these side effects, Krumholz says. “It’s my obligation, if I truly am a scientist, to have an open mind and learn if there’s something that can be done.”
SCIENCE FIRST wrote about these health concerns in January 2022, describing efforts by scientists at the National Institutes of Health to study and treat affected individuals. A study including 23 people was posted as a preprint in May 2022 but never published. Following Science’s story, almost 200 people contacted the journal sharing their postvaccination symptoms.
Research has since proceeded slowly. This is “a challenging outcome to monitor,” Tom Shimabukuro of the U.S. Centers for Disease Control and Prevention told a government advisory committee in January. Still, more than two dozen case studies have accumulated describing POTS or small fiber neuropathy following a COVID-19 shot, regardless of the vaccine manufacturer.
In 2021, Sujana Reddy, now an internal medicine resident physician at East Alabama Health, published a case study of postvaccine POTS in a 42-year-old man. She then heard from more than 250 people describing similar health concerns. Reddy began a study documenting POTS cases, not yet published, which now includes 55 people who developed symptoms 1 to 2 weeks after vaccination.
Another team scanned for postvaccine POTS across a specific population. Researchers led by cardiologists Alan Kwan and Susan Cheng at Cedars-Sinai Medical Center analyzed a health database of almost 285,000 people in the Los Angeles area; all had received at least one COVID-19 shot. They found that within 90 days after a shot, the rate of POTS-related symptoms was about 33% higher than in the 3 months before; 2581 people were diagnosed with POTS-related symptoms after vaccination, compared with 1945 beforehand. However, the study found a bigger effect from COVID-19 itself: The rate of POTS symptoms in about 12,000 unvaccinated people after infection was 52% higher than beforehand. Although Kwan cautions against extrapolating these numbers to a wider population, he says the pattern is intriguing. “Our data show a relatively clear signal that there probably is an increase in POTS after vaccination and after infection,” he says.
Others find the study compelling. “Even last year I was a little bit cautious” about the link between POTS and vaccination, says Tae Chung, a neuromuscular physiatrist who runs the POTS clinic at Johns Hopkins University. “I didn’t have quantitative data to back it up, but now I feel like I do.” Still, Chung stresses that this paper and other data also suggest COVID-19 vaccines protect against POTS and other Long Covid symptoms, and he remains a strong advocate for vaccination.
AN IMMUNE OVERREACTION to SARS-CoV-2 spike protein, which COVID-19 vaccines use to induce protective antibodies, is one possible cause of these symptoms. One theory is that after vaccination some people generate another round of antibodies targeting the first. Those antibodies could function somewhat like spike itself: Spike targets a cell surface protein called the angiotensin-converting enzyme 2 (ACE2) receptor, enabling the virus to enter cells. The rogue antibodies might also bind to ACE2, which helps regulate blood pressure and heart rate, says Bernhard Schieffer, a cardiologist at the University of Marburg. If those antibodies disrupt ACE2 signaling, that could cause the racing heart rates and blood pressure swings seen in POTS.
Small fiber neurons also have the ACE2 receptor on their surface, so in theory rogue antibodies could contribute to neuropathy. But Matthew Schelke, a neurologist at Columbia University who has treated small fiber neuropathy in both Long Covid and postvaccine patients, says pinning down a connection won’t be easy. Even when unusual antibodies turn up in someone’s blood, “it’s extremely difficult to know if any of these are pathogenic or if they are just bystanders,” he says. Other immune system components that fuel inflammation may also harm nerves, he notes.
Some people appear susceptible to complications after both infection and vaccination, a double vulnerability that can put them in an agonizing situation—eschewing more vaccine doses, often on the advice of their doctors, but also fearing the hazards of Long Covid. Reddy falls into this category. She caught the virus in early 2020 while caring for an infected patient and developed Long Covid, including POTS. Her symptoms dramatically worsened after her first vaccine dose.
An emergency medicine physician in New York City, Saleena Subaiya, experienced the same phenomenon in reverse. Within 24 hours of the second dose of COVID-19 vaccine in January 2021, they developed severe cognitive impairment, fatigue, and a loss of balance. Subaiya improved somewhat over the next year, but was forced to switch to a part-time research job. Then in December 2021, they were hit by Omicron and relapsed.
Postvaccination illness is “a long, relentless disease,” says Lawrence Purpura, an infectious disease specialist at Columbia University who is also Subaiya’s partner—and who treats both Long Covid patients and those with chronic symptoms after vaccination.
A DIAGNOSIS OF POTS or small fiber neuropathy post-vaccination can guide treatment. In POTS, doctors focus on increasing salt and fluid intake to boost blood volume and maintain blood pressure. Beta blockers, which slow racing hearts, may also help.
Small fiber neuropathy is treated with various medications to manage symptoms, and for severe cases sometimes intravenous immunoglobulin (IVIG), an expensive and hard-to-access antibody mixture that can tamp down immune overreactions. Some case studies report that IVIG helped people with postvaccine small fiber neuropathy, at least temporarily.
A more radical approach is plasma exchange, which is sometimes used for autoimmune disorders. Here the patient’s plasma—the liquid part of the blood containing antibodies and proteins—is separated from the blood cells and discarded. The blood cells are then returned to the patient along with a replacement liquid.
Plasma exchange helped a man who developed small fiber neuropathy following his second dose of a COVID-19 vaccine, Schelke and colleagues reported in October 2022 in Muscle & Nerve. “He responded very well,” with months of improvement, Schelke says, but recently returned with worsening symptoms.
Schieffer, meanwhile, has developed an experimental treatment regime that he says showed promise in an unpublished study of eight Long Covid and eight postvaccine patients. It includes statins, which can blunt inflammation in the circulatory system; and angiotensin II type 1 receptor blockers, which can help block the ACE2 pathway activation that may be dysregulated in patients. Schieffer and colleagues are hoping to start a clinical trial of the therapies with 500 people who have either Long Covid or postvaccine symptoms.
Patient advocates are trying to spur new studies. In the next few months, the nonprofit REACT19 plans to distribute small grants, in the tens of thousands of dollars, to teams studying immunology, biomarkers, and other features of postvaccine illness.
Even modest support matters, Krumholz says, because “it’s incumbent on us to produce preliminary data” to win over funders with deep pockets. His and Iwasaki’s LISTEN project now has about 2000 participants, roughly 1000 with Long Covid and 750 with postvaccination symptoms, he says. (LISTEN also includes healthy controls.) He hopes to begin to release results later this summer.
As countries draft plans for a round of updated vaccines, some scientists theorize, reassuringly, that people whose immune systems accepted a previous shot without incident would be highly unlikely to experience immune dysfunction following a booster. But that doesn’t change the urgent need to help those suffering now, Reddy says. “We need to figure out why it’s happening to this subset of people. Why is it happening to them and not everyone else?”
***
EK 18 (8.10.2023): Don’t you mean long covid?
No. It looks like ongoing symptoms in the aftermath of an acute respiratory infection (ARI) may not be restricted to covid-19. Researchers have found that some people experience long term symptoms after infections such as colds, influenza, or pneumonia, just as they can after a bout of covid-19.1 But the experience of “brain fog” appears to be restricted …
Kaynak: https://www.bmj.com/content/383/bmj.p2336
Makale: Sixty seconds on . . . long cold
***
EK 19 (25.3.2024): Uzayan Kovid diye bir şey yoktur. Bu, gereksiz korkuya ve bazı durumlarda iyileşmeyi engelleyebilecek tedbirlere sebep oluyor.
“Uzayan Kovid” tabiri, maskeler gibi bir kenara atılmalıdır; bir yıl boyunca çeşitli şikayetler bildirenlerin durumu aslında gripten farklı değildir.
Queensland Health’ de 18 yaş ve üzeri 5.112 kişi üzerinde yapılan çalışmanın Barselona’da düzenlenecek 2024 Avrupa Klinik Mikrobiyoloji ve Enfeksiyon Hastalıkları Kongresi’nde sunulması bekleniyor.
***
EK 20 (25.3.2024): Uzayan Kovid diye bir şey yoktur. Bu, gereksiz korkuya ve bazı durumlarda iyileşmeyi engelleyebilecek tedbirlere sebep oluyor.
“Uzayan Kovid” tabiri, maskeler gibi bir kenara atılmalıdır; bir yıl boyunca çeşitli şikayetler bildirenlerin durumu aslında gripten farklı değildir.
Queensland Health’ de 18 yaş ve üzeri 5.112 kişi üzerinde yapılan çalışmanın Barselona’da düzenlenecek 2024 Avrupa Klinik Mikrobiyoloji ve Enfeksiyon Hastalıkları Kongresi’nde sunulması bekleniyor.
***
EK 21 (21.11.2024): Bilim dünyasının “Uzayan Kovid” teşhisi ile yetinmeyeceği belliydi. Bunun bir de gizli olanı varmış: Gizli Uzayan Kovid. Araştırmaya göre, görülme oranı da Uzayan Kovid’ in 3 mislinden de fazlaymış; %7′ ye karşı %22.8. Amerikalılar bilimde çok geriler. Türkçe literatürü takip etselerdi, Gizli Uzayan Kovid teşhisinin çok uzun zamandan beri Kovid Başlangıcı adıyla tanımlandığını görürlerdi.
Researchers report that a new AI tool enhances the diagnostic process, potentially identifying more individuals who need care.
Previous diagnostic studies estimated that 7 percent of the population suffers from long COVID. However, a new study using an AI tool developed by Mass General Brigham indicates a significantly higher rate of 22.8 percent.
The AI-based tool can sift through electronic health records to help clinicians identify cases of long COVID. The often-mysterious condition can encompass a litany of enduring symptoms, including fatigue, chronic cough, and brain fog after infection from SARS-CoV-2.
The algorithm used was developed by drawing de-identified patient data from the clinical records of nearly 300,000 patients across 14 hospitals and 20 community health centers in the Mass General Brigham system. The results, published in the journal Med, could identify more people who should be receiving care for this potentially debilitating condition.
“Our AI tool could turn a foggy diagnostic process into something sharp and focused, giving clinicians the power to make sense of a challenging condition,” said senior author Hossein Estiri, head of AI Research at the Center for AI and Biomedical Informatics of the Learning Healthcare System (CAIBILS) at MGB and an associate professor of medicine at Harvard Medical School. “With this work, we may finally be able to see long COVID for what it truly is — and more importantly, how to treat it.”
For the purposes of their study, Estiri and colleagues defined long COVID as a diagnosis of exclusion that is also infection-associated. That means the diagnosis could not be explained in the patient’s unique medical record but was associated with a COVID infection. In addition, the diagnosis needed to have persisted for two months or longer in a 12-month follow-up window.
Precision Phenotyping: A Novel Approach
The novel method developed by Estiri and colleagues, called “precision phenotyping,” sifts through individual records to identify symptoms and conditions linked to COVID-19 to track symptoms over time in order to differentiate them from other illnesses. For example, the algorithm can detect if shortness of breath results from pre-existing conditions like heart failure or asthma rather than long COVID. Only when every other possibility was exhausted would the tool flag the patient as having long COVID.
“Physicians are often faced with having to wade through a tangled web of symptoms and medical histories, unsure of which threads to pull, while balancing busy caseloads. Having a tool powered by AI that can methodically do it for them could be a game-changer,” said Alaleh Azhir, co-lead author and an internal medicine resident at Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system.
The new tool’s patient-centered diagnoses may also help alleviate biases built into current diagnostics for long COVID, said researchers, who noted diagnoses with the official ICD-10 diagnostic code for long COVID trend toward those with easier access to healthcare.
The researchers said their tool is about 3 percent more accurate than the data ICD-10 codes capture, while being less biased. Specifically, their study demonstrated that the individuals they identified as having long COVID mirror the broader demographic makeup of Massachusetts, unlike long COVID algorithms that rely on a single diagnostic code or individual clinical encounters, skewing results toward certain populations such as those with more access to care.
“This broader scope ensures that marginalized communities, often sidelined in clinical studies, are no longer invisible,” said Estiri.
Limitations and Future Directions
Limitations of the study and AI tool include the fact that health record data the algorithm uses to account for long COVID symptoms may be less complete than the data physicians capture in post-visit clinical notes. Another limitation was the algorithm did not capture the possible worsening of a prior condition that may have been a long COVID symptom. For example, if a patient had COPD that worsened before they developed COVID-19, the algorithm might have removed the episodes even if they were long COVID indicators. Declines in COVID-19 testing in recent years also makes it difficult to identify when a patient may have first gotten COVID-19.
The study was limited to patients in Massachusetts.
Future studies may explore the algorithm in cohorts of patients with specific conditions, like COPD or diabetes. The researchers also plan to release this algorithm publicly on open access so physicians and healthcare systems globally can use it in their patient populations.
In addition to opening the door to better clinical care, this work may lay the foundation for future research into the genetic and biochemical factors behind long COVID’s various subtypes. “Questions about the true burden of long COVID — questions that have thus far remained elusive — now seem more within reach,” said Estiri.
Reference: “Precision phenotyping for curating research cohorts of patients with unexplained post-acute sequelae of COVID-19” by Alaleh Azhir, Jonas Hügel, Jiazi Tian, Jingya Cheng, Ingrid V. Bassett, Douglas S. Bell, Elmer V. Bernstam, Maha R. Farhat, Darren W. Henderson, Emily S. Lau, Michele Morris, Yevgeniy R. Semenov, Virginia A. Triant, Shyam Visweswaran, Zachary H. Strasser, Jeffrey G. Klann, Shawn N. Murphy and Hossein Estiri, 8 November 2024, Med.
DOI: 10.1016/j.medj.2024.10.009
Support was given by the National Institutes of Health, National Institute of Allergy and Infectious Diseases (NIAID) R01AI165535, National Heart, Lung, and Blood Institute (NHLBI) OT2HL161847, and National Center for Advancing Translational Sciences (NCATS) UL1 TR003167, UL1 TR001881, and U24TR004111. J. Hügel’s work was partially funded by a fellowship within the IFI program of the German Academic Exchange Service (DAAD) and by the Federal Ministry of Education and Research (BMBF) as well by the German Research Foundation (426671079).
Kaynak: https://scitechdaily.com/scientists-uncover-hidden-long-covid-cases-tripling-previous-estimates/
***
EK 22 (8.12.2024): ÖZCAN YÜCEL
Covid aşıları bir çok ruhsal bozukluğa yol açıyor. Güney Kore’deki önde gelen araştırmacıların 2 milyon insanın verilerine dayanarak yaptığı bomba çalışma, insanların “aşı” enjekte edildikten sonra duygularının, kişiliklerinin, hislerinin, korkularının, stres seviyelerinin, ruhsal iyilik hallerinin ve genel bakış açılarının değiştiğini buldu. Çalışma, saygın Nature Dergisi’nde yayımlandı. Araştırmada, Kovid aşılarının depresyonda %68,3, anksiyete bozukluklarında %43,9 ve uyku bozukluklarında %93,4 oranında artışa neden olduğu bulundu.
Kaynak: https://www.nature.com/articles/s41380-024-02627-0
K: https://x.com/drozcanyucel/status/1865627897563656582
***