UZAYAN KOVİD NEDİR, KİMLERDE GÖRÜLÜR, BELİRTİLERİ NELERDİR

Dikkat: Yazının sonunda ek var!
***
Çağla ile Yeni Bir Gün programında KOVİD’ in klinik tablolarını ve yeni tarif edilen “Uzayan KOVİD” i konuştuk.
Seyretmek için tıklayın:
https://www.youtube.com/watch?v=A-QaJbIr9Fs K:
https://www.facebook.com/yenibirgunfox/
***
EK 3 (7.12.2021): “Uzayan Kovid’ den mustarip olduklarını iddia eden 27 bin katılımcı üzerinde yapılan Fransız araştırmasında, sadece yüzde 4’ünün önceden virüsle karşılaştığı tespit edildi. Kaynak: https://twitter.com/korcanayata/status/1467938493376643075?s=20
***
EK 4 (31.5.2022): Kapsamlı değerlendirmelerde, çoğu vakada belirtilerin sebepleri ortaya konamadı. Anormal sistemik immün aktivasyon veya kalıcı viral enfeksiyona ait delil bulunamadı. Antikor seviyeleri çok değişkendi. Uzayan Kovid’ in patogenezi belli değildir.
Kaynak: https://www.acpjournals.org/doi/10.7326/M21-4905
Makale adı: A Longitudinal Study of COVID-19 Sequelae and Immunity: Baseline Findings
***
EK 5 (4.8.2022): Long COVID Comes in Three Forms: Study
Scientists have found three types of long COVID, which have their own symptoms and seem to appear across several coronavirus variants, according to a new preprint study published on MedRxiv that hasn’t yet been peer-reviewed.
Long COVID has been hard to define due to its large number of symptoms, but researchers at King’s College London have identified three distinct profiles — with long-term symptoms focused on neurological, respiratory, or physical conditions. So far, they also found patterns among people infected with the original coronavirus strain, the Alpha variant, and the Delta variant.
“These data show clearly that post-COVID syndrome is not just one condition but appears to have several subtypes,” Claire Steves, PhD, one of the study authors and a senior clinical lecturer in King’s College London’s School of Life Course & Population Sciences, said in a statement.
“Understanding the root causes of these subtypes may help in finding treatment strategies,” she said. “Moreover, these data emphasize the need for long-COVID services to incorporate a personalized approach sensitive to the issues of each individual.”
They found that the largest group had a cluster of symptoms in the nervous system, such as fatigue, brain fog, and headaches. It was the most common subtype among the Alpha variant, which was dominant in winter 2020-2021, and the Delta variant, which was dominant in 2021.
The second group had respiratory symptoms, such as chest pain and severe shortness of breath, which could suggest lung damage, the researchers wrote. It was the largest cluster for the original coronavirus strain in spring 2020, when people were unvaccinated.
The third group included people who reported a diverse range of physical symptoms, including heart palpitations, muscle aches and pain, and changes to their skin and hair. This group had some of the “most severe and debilitating multi-organ symptoms,” the researchers wrote.
The researchers found that the subtypes were similar in vaccinated and unvaccinated people based on the variants investigated so far. But the data showed that the risk of long COVID was reduced by vaccination.
In addition, although the three subtypes were present in all the variants, other symptom clusters had subtle differences among the variants, such as symptoms in the stomach and intestines. The differences could be due to other things that changed during the pandemic, such as the time of year, social behaviors, and treatments, the researchers said.
“Machine learning approaches, such as clustering analysis, have made it possible to start exploring and identifying different profiles of post-COVID syndrome,” Marc Modat, PhD, who led the analysis and is a senior lecturer at King’s College London’s School of Biomedical Engineering & Imaging Sciences, said in the statement.
“This opens new avenues of research to better understand COVID-19 and to motivate clinical research that might mitigate the long-term effects of the disease,” he said.
Kaynak: https://www.medscape.com/viewarticle/978469?src=soc_tw_220803_mscpedt_news_mdscp_longcovid&faf=1
***
EK 6 (13.8.2022): BROWNSTONE INSTİTUTE “Mikroplastiklere, nanopartiküllere, maskelerdeki kimyasallara ve nazofaringeal testleredaha çok maruz kalma, Uzayan Kovid’ i tanımlayan semptomların çoğuna paraleldir.”
Kaynak: https://twitter.com/brownstoneinst/status/1558031118661722113
***
EK 7 (25.8.2022): Uzayan Kovid diğer post-viral durumlara benziyor. Kaynak: https://www.medscape.com/viewarticle/979690 Makale: Long COVID Mimics Other Post-Viral Conditions
***
EK 8 (3.12.2022): Association of Initial SARS-CoV-2 Test Positivity With Patient-Reported Well-being 3 Months After a Symptomatic Illness
In this study, participants in both the COVID-19–positive and COVID-19–negative groups reported persistently poor physical, mental, or social well-being at 3-month follow-up. Although some individuals had clinically meaningful improvements over time, many reported moderate to severe impairments in well-being 3 months later. These results highlight the importance of including a control group of participants with negative COVID-19 results for comparison when examining the sequelae of COVID-19.
Kaynak: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2799116
***
EK 9 (7.2.2023): Kovid’den önce sağlıklı hayat tarzı uzayan Kovid riskinin azalmasıyla ilişkili bulundu.
Makale: Adherence to Healthy Lifestyle Prior to Infection and Risk of Post–COVID-19 Condition
Kaynak: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2800885
***
EK 10 (31.3.2023): The persistent symptoms and disability that characterize PCC are associated with factors other than SARS-CoV-2 infection, including psychosocial factors. This finding raises questions about the utility of the World Health Organization case definition and has implications for the planning of health care services as well as for further research on PCC.
Kaynak: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2802893
Makale: Prevalence and Characteristics Associated With Post–COVID-19 Condition Among Nonhospitalized Adolescents and Young Adults
***
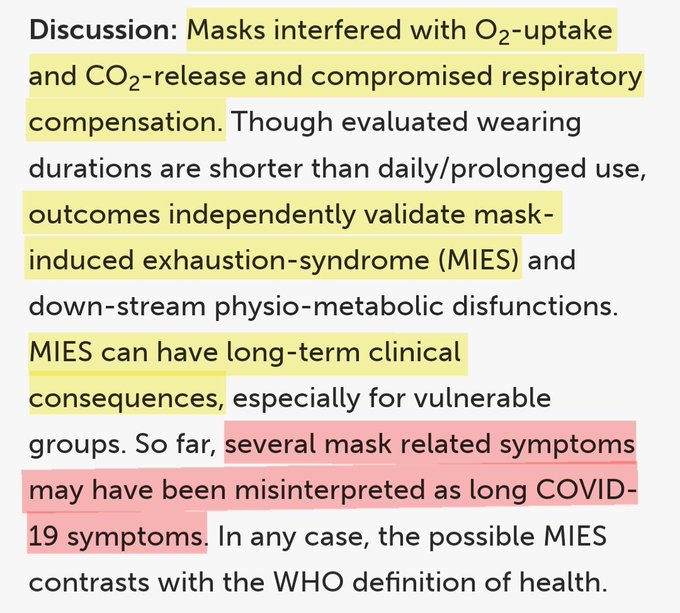
EK 11 (11.4.2023):Long Kovid (Uzayan Kovid) aslında maske takmanın bir neticesi olabilir.
Kaynak: https://twitter.com/drahmetrasim/status/1645907720929943552?s=20
***
EK 12 (6.6.2023): Kovid enfeksiyonundan önce kaygı ve depresyona sahip olmak uzayan Kovid riskini artırıyor. Bir enfeksiyondan sonra anksiyete ve depresyon geliştiren uzayan Kovid’ li kişilerde beyin bağlantısının bozulmasının yanı sıra hafıza, duygu ve diğer işlevleri düzenleyen alanlarda beyin küçülmesi olabilir.
Kaynak: https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2796097
Makale: Associations of Depression, Anxiety, Worry, Perceived Stress, and Loneliness Prior to Infection With Risk of Post–COVID-19 Conditions
***
EK 13 (4.7.2023): Rare link between coronavirus vaccines and Long Covid–like illness starts to gain acceptance Studies probe unusual cases of neurologic complications, blood pressure swings, and other side effects
COVID-19 vaccines have saved millions of lives, and the world is gearing up for a new round of boosters. But like all vaccines, those targeting the coronavirus can cause side effects in some people, including rare cases of abnormal blood clotting and heart inflammation. Another apparent complication, a debilitating suite of symptoms that resembles Long Covid, has been more elusive, its link to vaccination unclear and its diagnostic features ill-defined. But in recent months, what some call Long Vax has gained wider acceptance among doctors and scientists, and some are now working to better understand and treat its symptoms.
“You see one or two patients and you wonder if it’s a coincidence,” says Anne Louise Oaklander, a neurologist and researcher at Harvard Medical School. “But by the time you’ve seen 10, 20,” she continues, trailing off. “Where there’s smoke, there’s fire.”
Cases seem very rare—far less common than Long Covid after infection. Symptoms can include persistent headaches, severe fatigue, and abnormal heart rate and blood pressure. They appear hours, days, or weeks after vaccination and are difficult to study. But researchers and clinicians are increasingly finding some alignment with known medical conditions. One is small fiber neuropathy, a condition Oaklander studies, in which nerve damage can cause tingling or electric shock–like sensations, burning pain, and blood circulation problems. The second is a more nebulous syndrome, with symptoms sometimes triggered by small fiber neuropathy, called postural orthostatic tachycardia syndrome (POTS). It can involve muscle weakness, swings in heart rate and blood pressure, fatigue, and brain fog.
Patients with postvaccination symptoms may have features of one or both conditions, even if they don’t meet the criteria for a diagnosis. Both are also common in patients with Long Covid, where they’re often attributed to an immune overreaction.
Although more researchers are now taking Long Vax seriously, regulators in the United States and Europe say they have looked for, but have not found, a connection between COVID-19 vaccines and small fiber neuropathy or POTS. “We can’t rule out rare cases,” says Peter Marks, director of the U.S. Food and Drug Administration’s Center for Biologics Evaluation and Research, which oversees vaccines. “If a provider has somebody in front of them, they may want to take seriously the concept [of] a vaccine side effect,” he says. But Marks also worries about “the sensational headline” that could mislead the public, and he emphasizes that vaccine benefits far outweigh any risks.
Despite the uncertainties, German Minister of Health Karl Lauterbach acknowledged in March that though rare, Long Covid–like symptoms after vaccination are a real phenomenon. He said his ministry was working to organize funding for studies, although none has been announced so far.
Researchers studying these complications also worry about undermining trust in COVID-19 vaccines. Harlan Krumholz, a cardiologist at Yale University, says concern that the antivaccine movement would seize on any research findings made him hesitant at first to dive in. But about a year ago he and Yale immunologist Akiko Iwasaki began to welcome postvaccination patients into a new study called LISTEN that also includes Long Covid patients. Among other things, it aims to correlate symptoms with immune cell patterns in blood samples.
“I’m persuaded that there’s something going on” with these side effects, Krumholz says. “It’s my obligation, if I truly am a scientist, to have an open mind and learn if there’s something that can be done.”
SCIENCE FIRST wrote about these health concerns in January 2022, describing efforts by scientists at the National Institutes of Health to study and treat affected individuals. A study including 23 people was posted as a preprint in May 2022 but never published. Following Science’s story, almost 200 people contacted the journal sharing their postvaccination symptoms.
Research has since proceeded slowly. This is “a challenging outcome to monitor,” Tom Shimabukuro of the U.S. Centers for Disease Control and Prevention told a government advisory committee in January. Still, more than two dozen case studies have accumulated describing POTS or small fiber neuropathy following a COVID-19 shot, regardless of the vaccine manufacturer.
In 2021, Sujana Reddy, now an internal medicine resident physician at East Alabama Health, published a case study of postvaccine POTS in a 42-year-old man. She then heard from more than 250 people describing similar health concerns. Reddy began a study documenting POTS cases, not yet published, which now includes 55 people who developed symptoms 1 to 2 weeks after vaccination.
Another team scanned for postvaccine POTS across a specific population. Researchers led by cardiologists Alan Kwan and Susan Cheng at Cedars-Sinai Medical Center analyzed a health database of almost 285,000 people in the Los Angeles area; all had received at least one COVID-19 shot. They found that within 90 days after a shot, the rate of POTS-related symptoms was about 33% higher than in the 3 months before; 2581 people were diagnosed with POTS-related symptoms after vaccination, compared with 1945 beforehand. However, the study found a bigger effect from COVID-19 itself: The rate of POTS symptoms in about 12,000 unvaccinated people after infection was 52% higher than beforehand. Although Kwan cautions against extrapolating these numbers to a wider population, he says the pattern is intriguing. “Our data show a relatively clear signal that there probably is an increase in POTS after vaccination and after infection,” he says.
Others find the study compelling. “Even last year I was a little bit cautious” about the link between POTS and vaccination, says Tae Chung, a neuromuscular physiatrist who runs the POTS clinic at Johns Hopkins University. “I didn’t have quantitative data to back it up, but now I feel like I do.” Still, Chung stresses that this paper and other data also suggest COVID-19 vaccines protect against POTS and other Long Covid symptoms, and he remains a strong advocate for vaccination.
AN IMMUNE OVERREACTION to SARS-CoV-2 spike protein, which COVID-19 vaccines use to induce protective antibodies, is one possible cause of these symptoms. One theory is that after vaccination some people generate another round of antibodies targeting the first. Those antibodies could function somewhat like spike itself: Spike targets a cell surface protein called the angiotensin-converting enzyme 2 (ACE2) receptor, enabling the virus to enter cells. The rogue antibodies might also bind to ACE2, which helps regulate blood pressure and heart rate, says Bernhard Schieffer, a cardiologist at the University of Marburg. If those antibodies disrupt ACE2 signaling, that could cause the racing heart rates and blood pressure swings seen in POTS.
Small fiber neurons also have the ACE2 receptor on their surface, so in theory rogue antibodies could contribute to neuropathy. But Matthew Schelke, a neurologist at Columbia University who has treated small fiber neuropathy in both Long Covid and postvaccine patients, says pinning down a connection won’t be easy. Even when unusual antibodies turn up in someone’s blood, “it’s extremely difficult to know if any of these are pathogenic or if they are just bystanders,” he says. Other immune system components that fuel inflammation may also harm nerves, he notes.
Some people appear susceptible to complications after both infection and vaccination, a double vulnerability that can put them in an agonizing situation—eschewing more vaccine doses, often on the advice of their doctors, but also fearing the hazards of Long Covid. Reddy falls into this category. She caught the virus in early 2020 while caring for an infected patient and developed Long Covid, including POTS. Her symptoms dramatically worsened after her first vaccine dose.
An emergency medicine physician in New York City, Saleena Subaiya, experienced the same phenomenon in reverse. Within 24 hours of the second dose of COVID-19 vaccine in January 2021, they developed severe cognitive impairment, fatigue, and a loss of balance. Subaiya improved somewhat over the next year, but was forced to switch to a part-time research job. Then in December 2021, they were hit by Omicron and relapsed.
Postvaccination illness is “a long, relentless disease,” says Lawrence Purpura, an infectious disease specialist at Columbia University who is also Subaiya’s partner—and who treats both Long Covid patients and those with chronic symptoms after vaccination.
A DIAGNOSIS OF POTS or small fiber neuropathy post-vaccination can guide treatment. In POTS, doctors focus on increasing salt and fluid intake to boost blood volume and maintain blood pressure. Beta blockers, which slow racing hearts, may also help.
Small fiber neuropathy is treated with various medications to manage symptoms, and for severe cases sometimes intravenous immunoglobulin (IVIG), an expensive and hard-to-access antibody mixture that can tamp down immune overreactions. Some case studies report that IVIG helped people with postvaccine small fiber neuropathy, at least temporarily.
A more radical approach is plasma exchange, which is sometimes used for autoimmune disorders. Here the patient’s plasma—the liquid part of the blood containing antibodies and proteins—is separated from the blood cells and discarded. The blood cells are then returned to the patient along with a replacement liquid.
Plasma exchange helped a man who developed small fiber neuropathy following his second dose of a COVID-19 vaccine, Schelke and colleagues reported in October 2022 in Muscle & Nerve. “He responded very well,” with months of improvement, Schelke says, but recently returned with worsening symptoms.
Schieffer, meanwhile, has developed an experimental treatment regime that he says showed promise in an unpublished study of eight Long Covid and eight postvaccine patients. It includes statins, which can blunt inflammation in the circulatory system; and angiotensin II type 1 receptor blockers, which can help block the ACE2 pathway activation that may be dysregulated in patients. Schieffer and colleagues are hoping to start a clinical trial of the therapies with 500 people who have either Long Covid or postvaccine symptoms.
Patient advocates are trying to spur new studies. In the next few months, the nonprofit REACT19 plans to distribute small grants, in the tens of thousands of dollars, to teams studying immunology, biomarkers, and other features of postvaccine illness.
Even modest support matters, Krumholz says, because “it’s incumbent on us to produce preliminary data” to win over funders with deep pockets. His and Iwasaki’s LISTEN project now has about 2000 participants, roughly 1000 with Long Covid and 750 with postvaccination symptoms, he says. (LISTEN also includes healthy controls.) He hopes to begin to release results later this summer.
As countries draft plans for a round of updated vaccines, some scientists theorize, reassuringly, that people whose immune systems accepted a previous shot without incident would be highly unlikely to experience immune dysfunction following a booster. But that doesn’t change the urgent need to help those suffering now, Reddy says. “We need to figure out why it’s happening to this subset of people. Why is it happening to them and not everyone else?”
***
EK 14 (8.10.2023): Don’t you mean long covid?
No. It looks like ongoing symptoms in the aftermath of an acute respiratory infection (ARI) may not be restricted to covid-19. Researchers have found that some people experience long term symptoms after infections such as colds, influenza, or pneumonia, just as they can after a bout of covid-19.1 But the experience of “brain fog” appears to be restricted …
Kaynak: https://www.bmj.com/content/383/bmj.p2336
Makale: Sixty seconds on . . . long cold
***
EK 15 (25.3.2024): Uzayan Kovid diye bir şey yoktur. Bu, gereksiz korkuya ve bazı durumlarda iyileşmeyi engelleyebilecek tedbirlere sebep oluyor.
“Uzayan Kovid” tabiri, maskeler gibi bir kenara atılmalıdır; bir yıl boyunca çeşitli şikayetler bildirenlerin durumu aslında gripten farklı değildir.
Queensland Health’ de 18 yaş ve üzeri 5.112 kişi üzerinde yapılan çalışmanın Barselona’da düzenlenecek 2024 Avrupa Klinik Mikrobiyoloji ve Enfeksiyon Hastalıkları Kongresi’nde sunulması bekleniyor.
***
EK 16 (21.11.2024): Bilim dünyasının “Uzayan Kovid” teşhisi ile yetinmeyeceği belliydi. Bunun bir de gizli olanı varmış: Gizli Uzayan Kovid. Araştırmaya göre, görülme oranı da Uzayan Kovid’ in 3 mislinden de fazlaymış; %7′ ye karşı %22.8. Amerikalılar bilimde çok geriler. Türkçe literatürü takip etselerdi, Gizli Uzayan Kovid teşhisinin çok uzun zamandan beri Kovid Başlangıcı adıyla tanımlandığını görürlerdi.
Researchers report that a new AI tool enhances the diagnostic process, potentially identifying more individuals who need care.
Previous diagnostic studies estimated that 7 percent of the population suffers from long COVID. However, a new study using an AI tool developed by Mass General Brigham indicates a significantly higher rate of 22.8 percent.
The AI-based tool can sift through electronic health records to help clinicians identify cases of long COVID. The often-mysterious condition can encompass a litany of enduring symptoms, including fatigue, chronic cough, and brain fog after infection from SARS-CoV-2.
The algorithm used was developed by drawing de-identified patient data from the clinical records of nearly 300,000 patients across 14 hospitals and 20 community health centers in the Mass General Brigham system. The results, published in the journal Med, could identify more people who should be receiving care for this potentially debilitating condition.
“Our AI tool could turn a foggy diagnostic process into something sharp and focused, giving clinicians the power to make sense of a challenging condition,” said senior author Hossein Estiri, head of AI Research at the Center for AI and Biomedical Informatics of the Learning Healthcare System (CAIBILS) at MGB and an associate professor of medicine at Harvard Medical School. “With this work, we may finally be able to see long COVID for what it truly is — and more importantly, how to treat it.”
For the purposes of their study, Estiri and colleagues defined long COVID as a diagnosis of exclusion that is also infection-associated. That means the diagnosis could not be explained in the patient’s unique medical record but was associated with a COVID infection. In addition, the diagnosis needed to have persisted for two months or longer in a 12-month follow-up window.
Precision Phenotyping: A Novel Approach
The novel method developed by Estiri and colleagues, called “precision phenotyping,” sifts through individual records to identify symptoms and conditions linked to COVID-19 to track symptoms over time in order to differentiate them from other illnesses. For example, the algorithm can detect if shortness of breath results from pre-existing conditions like heart failure or asthma rather than long COVID. Only when every other possibility was exhausted would the tool flag the patient as having long COVID.
“Physicians are often faced with having to wade through a tangled web of symptoms and medical histories, unsure of which threads to pull, while balancing busy caseloads. Having a tool powered by AI that can methodically do it for them could be a game-changer,” said Alaleh Azhir, co-lead author and an internal medicine resident at Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system.
The new tool’s patient-centered diagnoses may also help alleviate biases built into current diagnostics for long COVID, said researchers, who noted diagnoses with the official ICD-10 diagnostic code for long COVID trend toward those with easier access to healthcare.
The researchers said their tool is about 3 percent more accurate than the data ICD-10 codes capture, while being less biased. Specifically, their study demonstrated that the individuals they identified as having long COVID mirror the broader demographic makeup of Massachusetts, unlike long COVID algorithms that rely on a single diagnostic code or individual clinical encounters, skewing results toward certain populations such as those with more access to care.
“This broader scope ensures that marginalized communities, often sidelined in clinical studies, are no longer invisible,” said Estiri.
Limitations and Future Directions
Limitations of the study and AI tool include the fact that health record data the algorithm uses to account for long COVID symptoms may be less complete than the data physicians capture in post-visit clinical notes. Another limitation was the algorithm did not capture the possible worsening of a prior condition that may have been a long COVID symptom. For example, if a patient had COPD that worsened before they developed COVID-19, the algorithm might have removed the episodes even if they were long COVID indicators. Declines in COVID-19 testing in recent years also makes it difficult to identify when a patient may have first gotten COVID-19.
The study was limited to patients in Massachusetts.
Future studies may explore the algorithm in cohorts of patients with specific conditions, like COPD or diabetes. The researchers also plan to release this algorithm publicly on open access so physicians and healthcare systems globally can use it in their patient populations.
In addition to opening the door to better clinical care, this work may lay the foundation for future research into the genetic and biochemical factors behind long COVID’s various subtypes. “Questions about the true burden of long COVID — questions that have thus far remained elusive — now seem more within reach,” said Estiri.
Reference: “Precision phenotyping for curating research cohorts of patients with unexplained post-acute sequelae of COVID-19” by Alaleh Azhir, Jonas Hügel, Jiazi Tian, Jingya Cheng, Ingrid V. Bassett, Douglas S. Bell, Elmer V. Bernstam, Maha R. Farhat, Darren W. Henderson, Emily S. Lau, Michele Morris, Yevgeniy R. Semenov, Virginia A. Triant, Shyam Visweswaran, Zachary H. Strasser, Jeffrey G. Klann, Shawn N. Murphy and Hossein Estiri, 8 November 2024, Med.
DOI: 10.1016/j.medj.2024.10.009
Support was given by the National Institutes of Health, National Institute of Allergy and Infectious Diseases (NIAID) R01AI165535, National Heart, Lung, and Blood Institute (NHLBI) OT2HL161847, and National Center for Advancing Translational Sciences (NCATS) UL1 TR003167, UL1 TR001881, and U24TR004111. J. Hügel’s work was partially funded by a fellowship within the IFI program of the German Academic Exchange Service (DAAD) and by the Federal Ministry of Education and Research (BMBF) as well by the German Research Foundation (426671079).
Kaynak: https://scitechdaily.com/scientists-uncover-hidden-long-covid-cases-tripling-previous-estimates/
***












Bu yazıdaki resim herhalde eski olmalı çünkü videodaki gömlek kravat farklı. Bizden kaçmaz hocam?